Autovent: Difference between revisions
Jump to navigation
Jump to search
mNo edit summary |
|||
| Line 35: | Line 35: | ||
* Reassess and document breath sounds every 10 minutes or when change in the patient’s chief complaint, level of consciousness, airway, breathing, circulation, and vital signs to ensure that endotracheal tube is still in proper position. | * Reassess and document breath sounds every 10 minutes or when change in the patient’s chief complaint, level of consciousness, airway, breathing, circulation, and vital signs to ensure that endotracheal tube is still in proper position. | ||
[[Category:Procedure Guidelines]] | [[Category:Procedure Guidelines|0901]] | ||
Latest revision as of 17:38, 1 February 2018
Procedure Guidelines
9.01 AUTOVENT
INDICATIONS:
- To provide ventilatory support in the intubated adult patient during interfacility transfers.
- To assist ventilations in the intubated medical patient.
CONTRAINDICATIONS:
- Trauma patients.
- Pediatric patients (under 8 years of age and 70 lbs. Or less).
EQUIPMENT:
- Oxygen supply with greater than 500 psi.
- Stethoscope.
- Bag Valve Mask for ventilatory backup.
- Suction on stand-by.
PROCEDURE:
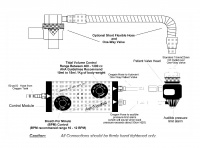
- Connect the oxygen high-pressure line to the quick-connect Oxygen adapter. Connect (Hand tighten) the other end to the gas inlet of the control module.
- Connect (Hand tighten) the Patient Valve Supply tubing to the Patient Valve outlets of the control module.
- After initial control module settings have been made, connect the patient Valve Assembly directly to the endotracheal tube adapter.
- During interfacility transfers, maintain the BPM and Tidal Volume settings per physician orders.
MONITOR:
- Assess the following parameters immediately after connecting the patient to the ventilator:
- Breaths Per Minute (BPM), adjust the BPM control knob to maintain an adequate ventilator rate. Average adult settings are greater than or equal to 12 BPM.
- Tidal Volume, adjust for adequate bilateral chest rise and fall to maintain an adequate ventilatory depth. Average adult settings are between 400 to 1,000 ml.
- Auscultate for the presence of bilateral breath sounds and the absence of abdominal sounds.
- Reassess and document breath sounds every 10 minutes or when change in the patient’s chief complaint, level of consciousness, airway, breathing, circulation, and vital signs to ensure that endotracheal tube is still in proper position.