Selective Spinal Immobilization: Difference between revisions
| Line 65: | Line 65: | ||
'''''WHEN IN DOUBT, TREAT AS SPINAL INJURY''''' | '''''WHEN IN DOUBT, TREAT AS SPINAL INJURY''''' | ||
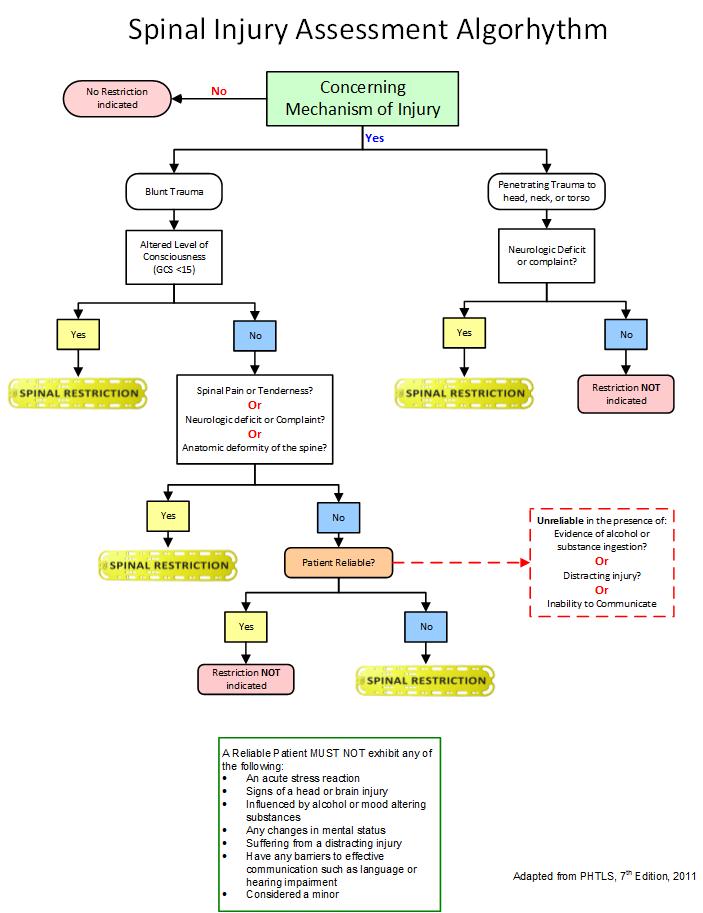
[[File:Selective_Spinal_Flowchart_rev_1.jpg]] | |||
Revision as of 12:40, 1 August 2013
Section 6 - TRAUMA
6.03 SELECTIVE SPINAL IMMOBILIZATION
Background: This parameter is intended to provide personnel with a guideline for the selective exclusion from spinal restriction on patients who have a low index of suspicion mechanism of injury for spinal injury combined with a thorough assessment that supports the exclusion.
Goal: Patients will be assessed for the need for spinal restriction based on clear clinical criteria. Any patient presenting with a positive or questionable mechanism-of-injury (MOI) that indicates the potential for spinal injury, and for whom it is not possible to clinically rule-out the need, will have spinal restriction performed. Personnel must document all pertinent findings consistent with their assessment of the patient’s need, or lack of need, for restriction.
Supportive References:
- Advanced Trauma Life Support (ATLS) for Doctors (2008 Edition):
- General Management of Immobilization; Chapter 7; page 168
- “Proper immobilization [of the spine] is achieved with the patient in neutral position – that is, supine without rotating or bending the spinal column. No effort should be made to reduce an obvious deformity.”
- “Attempts to align the spine for the purpose of immobilization on the backboard are not recommended if they cause pain.”
- Guidelines for Screening Patients with suspected Spine Injury; Chapter 7, Page 169
- “Patients who are awake, alert, sober, and neurologically normal, and have no neck pain or midline tenderness: These patients are extremely unlikely to have an acute c-spine fracture or instability.”
- General Management of Immobilization; Chapter 7; page 168
- Prehospital Trauma Life support (PHTLS), Seventh Edition (2011):
- Manual In-line Stabilization of the Head; Chapter 10; page 259
- “Neutral in-line movement should not be attempted if a patient’s injuries are so severe that the head presents in such misalignment that it no longer appears to extend from the midline of the shoulders. In these situations, the patient’s head must be immobilized in the position in which it was initially found.”
- Guidelines for Rigid Cervical Collars; Figure 10-14; page 259
- Rigid Cervical Collars “must not inhibit a patient’s ability to open the mouth or the prehospital care provider’s ability to open the mouth if vomiting occurs.”
- Rigid Cervical Collars “should not obstruct or hinder ventilation in any way.”
- Manual In-line Stabilization of the Head; Chapter 10; page 259
General Guidelines for the Proper Management of Spinal Restriction:
- When spinal restriction is considered or utilized it MUST NOT:
- Cause further harm
- Cause further or increased pain
- Compromise the airway
- Compromise ventilation efforts
- Manipulate or move broken bones
- Increase the risk of soft tissue breakdown or pressure points in susceptible patients
- Spinal restriction definition:
- At a minimum advise the reliable/cooperative patient not to move
- If the patient is able to tolerate a cervical collar, one must be applied
- Secure the patient on the ambulance stretcher for transport.
- Spinal packaging definition:
- Secure manual cervical immobilization
- Place a cervical collar on the patient
- Secure the patient to a long backboard as long as it does not deteriorate the patient’s condition.
Spinal Injury Assessment Criteria:
- Consider Mechanism of Injury
- Positive mechanism → Apply c-collar, consider full spinal restriction
- Negative mechanism → Negative for spinal injury, no spinal restriction required
- Uncertain mechanism → Continue assessment
- Assess for spine pain and/or tenderness. If assessment reveals:
- Positive pain/tenderness →complete spinal restriction required
- Negative response regarding pain/tenderness → begin motor sensory exam
- Perform motor/sensory exam
- Motor exam upper and lower extremities
- Sensory exam on all extremities
- Presence/absence of abnormal sensation
- Pain sensation in upper or lower extremities
- Perform reliable patient exam
- Is the patient exhibiting any of the following:
- Acute stress reaction
- Brain/head injury
- Intoxication
- Altered mental status
- Suffering a distracting injury
- Communications barriers – language, hearing impairment, toddlers, infants
- Is the patient exhibiting any of the following:
- Abnormal Assessment – spinal restriction required
- Normal Assessment – Spinal restriction is NOT required
WHEN IN DOUBT, TREAT AS SPINAL INJURY