Continuous Positive Airway Pressure Device: Difference between revisions
mNo edit summary |
|||
| (2 intermediate revisions by the same user not shown) | |||
| Line 72: | Line 72: | ||
* Provide supportive BLS/ALS interventions as needed. | * Provide supportive BLS/ALS interventions as needed. | ||
* Paramedic should immediately notify Medical Control and ED staff upon arrival. | * Paramedic should immediately notify Medical Control and ED staff upon arrival. | ||
| Line 101: | Line 100: | ||
* Document vital signs every five minutes, include EtCO2 and SpO2. | * Document vital signs every five minutes, include EtCO2 and SpO2. | ||
* Complete CPAP QI Form | * Complete CPAP QI Form | ||
[[Category:Procedure Guidelines|0908]] | |||
Latest revision as of 17:40, 1 February 2018
Procedure Guidelines
9.08 CONTINUOUS POSITIVE AIRWAY PRESSURE DEVICE
Continuous Positive Airway Pressure (CPAP) has been shown to rapidly improve vital signs, gas exchange, the work of breathing, decrease the sense of dyspnea, and decrease the need for endotracheal intubation in the patients who suffer from COPD, pulmonary edema, CHF, and pneumonia. In patients with CHF, CPAP improves hemodynamics by reducing preload and afterload. CPAP maintains positive airway pressure above atmospheric pressure throughout inspiration and exhalation in order to increase the transpulmonary pressure gradient allowing gas to passively flow down into the smaller airways and alveoli, as well as preventing the bronchioles from collapsing.
NOTE: IN ORDER FOR CPAP TO BE USED, THE PATIENT MUST BE BREATHING.
INDICATIONS:
- Hypoxemia secondary to Congestive Heart Failure and Acute Cardiogenic Pulmonary Edema PRACTICE PARAMETER 4.11
- For relief of Hypoxemia and Shortness of Breath (SOB)/Dyspnea secondary to Pneumonia,
- Acute Asthma / COPD with wheezing – PRACTICE PARAMETER 3.01
- Carbon Monoxide Poisoning ( 5 cmH2O) – PRACTICE PARAMETER 3.02
- Near-drowning (10 cmH2O) – PRACTICE PARAMETER 6.08
CONTRAINDICATIONS:
- Penetrating chest trauma
- Severe hypotension
- Persistent nausea and or vomiting
- Unconscious or obtundation
- Respiratory / Cardiac arrest
- Patient unable to protect their own airway
- Agonal respirations
SIGNS AND SYMPTOMS:
- Dyspnea and tachypnea.
- Chest Pain, hypertension, tachycardia.
- Anxiety, restlessness, altered L.O.C.
- Rales, wheezes, frothy sputum (severe cases)
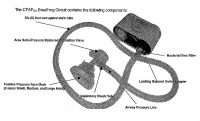
ASSEMBLE THE EQUIPMENT
- Do not bypass, delay or withhold conventional treatment while assembling or using the CPAP device.
- Connect the locking bayonet outlet adapter with the clear prongs perpendicular to the black prongs on the face of the CPAP machine. Push the circuit down to the rim of the black ports. Turn the circuit clockwise to lock it in place.
- Connect the oxygen tube to the 50psi inlet on the CPAP machine.(Be sure the control knob is still in the OFF position)
- Connect the other end of the oxygen tube to oxygen cylinder(minimum of 1000psi)
PROCEDURE:
- Assess Vital Signs
- Attach heart monitor and pulse oximeter
- Assemble the equipment as per Figure 1
- Patient requires “verbal sedation” to be used effectively.
Setting the desired CPAP level
- Open the cylinder. DO NOT turn on the FLOW. (Start CPAPos at ambient pressure ‘0’ cmH2O)
- To set the flow occlude the inlet and turn the black knob clockwise (at least one complete revolution) until the desired CPAP level is achieved.
- Instruct patient to hold mask, breath in through their nose slowly and exhale through their mouth as long as possible (count slowly and aloud to four then instruct to inhale slowly).
CAUTION: In some cases patient will have to be persuaded to place mask on to face. Offer reassurance. Example: Patient: “I can’t get air in!” Paramedic: “This will help you get air in.” “This will help you breath easier as the pressure on the machine is increased”.
- Explain to the patient that you will begin to slowly increase the pressure and to continue exhaling out against the pressure as long as possible before inhaling.
- Slowly titrate the pressure to the appropriate level:
- CHF/APE/NEAR DROWNING -10cmH2O
- COPD/CO POISONING - 5 cmH2O
- Once the desired CPAP level is achieved, connect the mask to the circuit.

Placing the mask on the patient:
Before placing the mask onto the patient’s face, place the Nasal EtCO2 on the patient, then assist the patient with sealing the mask to their face. (Be sure to cover the patient’s nose and mouth-tight seal-no leaks) Next use the black head gear to physically strap the mask to patient’s face.
COMPLICATIONS:
WARNING: Potential side effects of CPAP may include fluid retention, pneumothorax, decreased cardiac output and gastric distention.
- Stop treatment.
- Provide supportive BLS/ALS interventions as needed.
- Paramedic should immediately notify Medical Control and ED staff upon arrival.
HOSPITAL NOTIFICATION:
Notify hospital via radio that patient is on CPAP and request that Respiratory be notified.
MONITORING THE PATIENT:
- During operation, monitor the following periodically:
- Monitor to assure that there are no leaks at the patient connection.
- Monitor the Airway Pressure Gauge.
- Monitor SpO2
- Monitor B/P and EKG
- Monitor the patient’s breathing with chest auscultation
- Monitor the patient for signs of dehydration and discomfort in the upper airways
- Monitor the patient’s condition for improvement, including the respiratory rate, mental status and SpO2 percentage.
- If the patient’s condition is improving, continue to monitor the patient.
- If the patient’s condition is not improving, increase the oxygen adjustment valve. Titrate in increments of ½ turns q 2 minutes to SpO2 of 100%.
- If the patient’s condition is deteriorating despite increasing the oxygen adjustment valve, discontinue the CPAP device and prepare for orotracheal intubation.
- To turn the CPAPos unit off, disconnect the O2 supply hose from the source or turn off at the O2 cylinder.
DOCUMENTATION:
- The Paramedic attending a patient with CPAP will do the following;
- Document indications for CPAP.
- Document CPAP settings.
- Document Effects/Adverse reactions
- Document vital signs every five minutes, include EtCO2 and SpO2.
- Complete CPAP QI Form