Ventricular Fibrillation Pulseless Ventricular Tachycardia
Section 4 - CARDIAC
4.08 CARDIAC ARREST - VENTRICULAR FIBRILLATION /PULSELESS VENTRICULAR TACHYCARDIA
Ventricular Fibrillation (VF) and Pulseless V-Tach (VT) focuses in the correction of the dysrhythmia into a pulse producing rhythm. Consider all possible reversible causes for cardiac arrest utilizing a national recommended mnemonic of “H’s and T’s”:
| H’s | T’s |
|---|---|
| Hypovolemia | Tension Pneumothorax |
| Hypoxia | Tamponade, cardiac |
| Hydrogen Ion (acidosis) | Toxins or Tablets (overdose) |
| Hypo/hyperkalemia | Thrombosis, pulmonary |
| Hypothermia | Thrombosis, cardiac |
In addition, also consider the following:
| Hypoglycemia | Trauma |
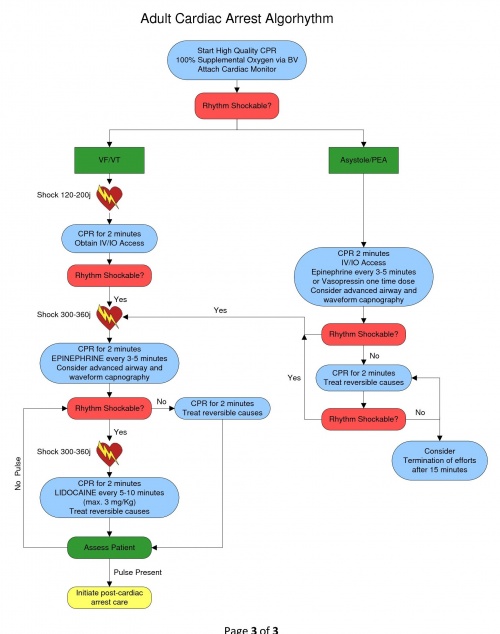
When the Patient found in cardiac arrest:
- Initiate BLS algorhythm with 5 cycles of high quality CPR (push hard/push fast)
- Minimum of 100 compressions per minute, minimize interruptions
- Compression rate of 30:2 for approximately 2 minutes
- Depth of compression of at least 2 inches
- Initiate the use of a mechanical compression device if available
- Assist ventilations with OXYGEN @ 100% via BVM - DO NOT HYPERVENTILATE
- Attach cardiac monitor – Evaluate the cardiac rhythm
- VF/VT Present – deliver a DEFIBRILLATION 120-200j biphasic
- Continue high quality CPR/Ventilations for 2 minutes
- Establish intravenous access via IV or IO
- Consider advanced airway procedure using supraglottic airway (king tube) or endotracheal intubation
- Do not interrupt compressions to place an advanced airway
- Confirm tube placement with capnography (a range 5-20 mmHg is indicative of low cardiac output)
- Administer EPINEPHRINE 1:10,000 1 mg IV / IO – repeat every 3-5 minutes of arrest
- Reassess for circulation every two minutes
- VF/VT Present – deliver a DEFIBRILLATION 300-360j biphasic
- Subsequent shocks should be at the higher dose selected
If after 3 attempts at defibrillation and patient is still presenting VF, consider using double sequential defibrillation for subsequent shocks at 720j biphasic. If two manual monitors are not available, use one monitor and one AED even though they will not be able to deliver full 720j. (using double sequential defibrillation)
- Administer antidysrhythmic medication:
- AMIODARONE 300 mg IVP, IO.
- May repeat second dose AMIODARONE (if needed) 150 mg IV, IO in 3-5 minutes.
- Maximum dose 450 mg.
- OR
- Administer LIDOCAINE 1 to 1.5 mg/kg IVP, IO. May repeat every 5-10 minutes to a maximum of 3 mg/Kg.
- In patients over age 70 or in those with known hepatic disease, administer LIDOCAINE gradually up to a full initial loading dose or until a maximum of 1.5 mg/kg administered.
- If VF/VT converts to a pulse-producing non-heart block supraventricular rhythm, administer a LIDOCAINE DRIP 1-4 mg/min.
- In patients over age 70 or in those with known hepatic disease, administer LIDOCAINE DRIP at the lower 1-2 mg/min. MONITOR FOR SIGNS OF TOXICITY including seizure activity.
- Administer MAGNESIUM SULFATE 2 gm IVP only if suspected Polymorphic VT (Torsades de pointes) or hypomagnesemic state (chronic alcohol, diuretic use)
- Administer SODIUM BICARBONATE 1 mEq/kg IVP if suspected, HYPERKALEMIA (e.g. dialysis patient), or Tricyclic antidepressant OD
If patient combative post resuscitation, refer to ANALGESIA / SEDATION PARAMETER (2.04)
Deliver all Defibrillations at 360 Joules in any patient who has had an Automatic Implanted Cardioverter Defibrillator (AICD) shock. (Use Anterior/Posterior position if possible for Defibrillator Pads - Do not place pads over device).
- Consider sedation in patient experiencing cardioversion or defibrillation by their own AICD.
- Leave copy of ECG at ER on any patient with implanted device.